InVivoPlus anti-mouse Ly6G
Product Details
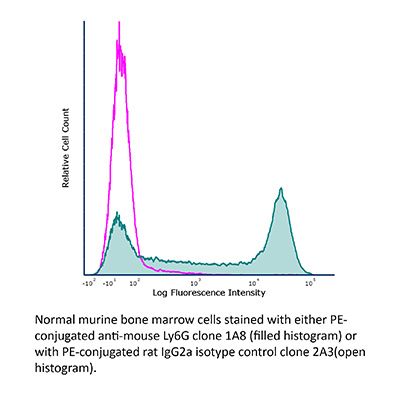
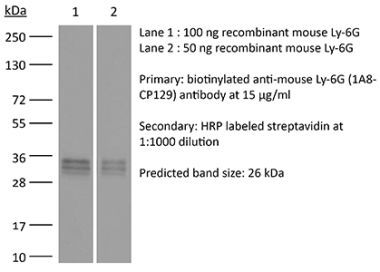
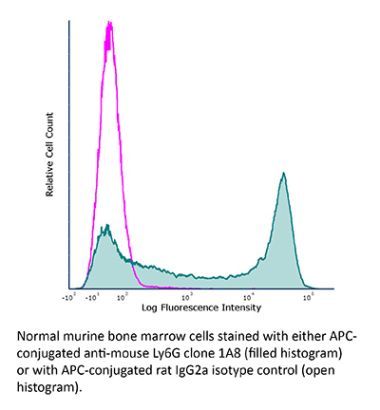
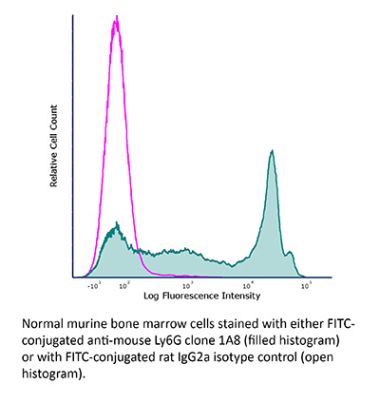
The 1A8 monoclonal antibody reacts with mouse Ly6G. Ly6G is a 21-25 kDa member of the Ly-6 superfamily of GPI-anchored cell surface proteins with roles in cell signaling and cell adhesion. Ly6G is expressed differentially during development by cells in the myeloid lineage including monocytes, macrophages, granulocytes, and neutrophils. Monocytes typically express Ly6G transiently during development while mature granulocytes and peripheral neutrophils retain expression making Ly6G a good cell surface marker for these populations. Unlike the RB6-8C5 antibody, the 1A8 antibody reacts specifically with mouse Ly6G with no reported cross reactivity with Ly6C.Specifications
| Isotype | Rat IgG2a, κ |
|---|---|
| Recommended Isotype Control(s) | InVivoPlus rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer |
| Conjugation | This product is unconjugated. Conjugation is available via our Antibody Conjugation Services. |
| Immunogen | EL4J cells transfected with Ly6G |
| Reported Applications |
in vivo neutrophil depletion in vivo MDSC depletion Immunofluorescence Immunohistochemistry (paraffin) Immunohistochemistry (frozen) Flow cytometry |
| Formulation |
PBS, pH 7.0 Contains no stabilizers or preservatives |
| Aggregation* |
<5% Determined by SEC |
| Purity |
>95% Determined by SDS-PAGE |
| Sterility | 0.2 µm filtration |
| Purification | Protein G |
| RRID | AB_1107721 |
| Molecular Weight | 150 kDa |
| Murine Pathogen Tests* |
Ectromelia/Mousepox Virus: Negative Hantavirus: Negative K Virus: Negative Lactate Dehydrogenase-Elevating Virus: Negative Lymphocytic Choriomeningitis virus: Negative Mouse Adenovirus: Negative Mouse Cytomegalovirus: Negative Mouse Hepatitis Virus: Negative Mouse Minute Virus: Negative Mouse Norovirus: Negative Mouse Parvovirus: Negative Mouse Rotavirus: Negative Mycoplasma Pulmonis: Negative Pneumonia Virus of Mice: Negative Polyoma Virus: Negative Reovirus Screen: Negative Sendai Virus: Negative Theiler’s Murine Encephalomyelitis: Negative |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
Additional Formats
Recommended Products
in vivo neutrophil depletion
Davis, R. W. t., et al. (2018). "Luminol Chemiluminescence Reports Photodynamic Therapy-Generated Neutrophil Activity In Vivo and Serves as a Biomarker of Therapeutic Efficacy" Photochem Photobiol . PubMed
Inflammatory cells, most especially neutrophils, can be a necessary component of the antitumor activity occurring after administration of photodynamic therapy. Generation of neutrophil responses has been suggested to be particularly important in instances when the delivered photodynamic therapy (PDT) dose is insufficient. In these cases, the release of neutrophil granules and engagement of antitumor immunity may play an important role in eliminating residual disease. Herein, we utilize in vivo imaging of luminol chemiluminescence to noninvasively monitor neutrophil activation after PDT administration. Studies were performed in the AB12 murine model of mesothelioma, treated with Photofrin-PDT. Luminol-generated chemiluminescence increased transiently 1 h after PDT, followed by a subsequent decrease at 4 h after PDT. The production of luminol signal was not associated with the influx of Ly6G(+) cells, but was related to oxidative burst, as an indicator of neutrophil function. Most importantly, greater levels of luminol chemiluminescence 1 h after PDT were prognostic of a complete response at 90 days after PDT. Taken together, this research supports an important role for early activity by Ly6G(+) cells in the generation of long-term PDT responses in mesothelioma, and it points to luminol chemiluminescence as a potentially useful approach for preclinical monitoring of neutrophil activation by PDT.
in vivo neutrophil depletion
Moynihan, K. D., et al. (2016). "Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses" Nat Med. doi : 10.1038/nm.4200. PubMed
Checkpoint blockade with antibodies specific for cytotoxic T lymphocyte-associated protein (CTLA)-4 or programmed cell death 1 (PDCD1; also known as PD-1) elicits durable tumor regression in metastatic cancer, but these dramatic responses are confined to a minority of patients. This suboptimal outcome is probably due in part to the complex network of immunosuppressive pathways present in advanced tumors, which are unlikely to be overcome by intervention at a single signaling checkpoint. Here we describe a combination immunotherapy that recruits a variety of innate and adaptive immune cells to eliminate large tumor burdens in syngeneic tumor models and a genetically engineered mouse model of melanoma; to our knowledge tumors of this size have not previously been curable by treatments relying on endogenous immunity. Maximal antitumor efficacy required four components: a tumor-antigen-targeting antibody, a recombinant interleukin-2 with an extended half-life, anti-PD-1 and a powerful T cell vaccine. Depletion experiments revealed that CD8+ T cells, cross-presenting dendritic cells and several other innate immune cell subsets were required for tumor regression. Effective treatment induced infiltration of immune cells and production of inflammatory cytokines in the tumor, enhanced antibody-mediated tumor antigen uptake and promoted antigen spreading. These results demonstrate the capacity of an elicited endogenous immune response to destroy large, established tumors and elucidate essential characteristics of combination immunotherapies that are capable of curing a majority of tumors in experimental settings typically viewed as intractable.
in vivo neutrophil depletion
Conde, P., et al. (2015). "DC-SIGN(+) Macrophages Control the Induction of Transplantation Tolerance" Immunity 42(6): 1143-1158. PubMed
Tissue effector cells of the monocyte lineage can differentiate into different cell types with specific cell function depending on their environment. The phenotype, developmental requirements, and functional mechanisms of immune protective macrophages that mediate the induction of transplantation tolerance remain elusive. Here, we demonstrate that costimulatory blockade favored accumulation of DC-SIGN-expressing macrophages that inhibited CD8(+) T cell immunity and promoted CD4(+)Foxp3(+) Treg cell expansion in numbers. Mechanistically, that simultaneous DC-SIGN engagement by fucosylated ligands and TLR4 signaling was required for production of immunoregulatory IL-10 associated with prolonged allograft survival. Deletion of DC-SIGN-expressing macrophages in vivo, interfering with their CSF1-dependent development, or preventing the DC-SIGN signaling pathway abrogated tolerance. Together, the results provide new insights into the tolerogenic effects of costimulatory blockade and identify DC-SIGN(+) suppressive macrophages as crucial mediators of immunological tolerance with the concomitant therapeutic implications in the clinic.
in vivo neutrophil depletion
Griseri, T., et al. (2015). "Granulocyte Macrophage Colony-Stimulating Factor-Activated Eosinophils Promote Interleukin-23 Driven Chronic Colitis" Immunity 43(1): 187-199. PubMed
The role of intestinal eosinophils in immune homeostasis is enigmatic and the molecular signals that drive them from protective to tissue damaging are unknown. Most commonly associated with Th2 cell-mediated diseases, we describe a role for eosinophils as crucial effectors of the interleukin-23 (IL-23)-granulocyte macrophage colony-stimulating factor (GM-CSF) axis in colitis. Chronic intestinal inflammation was characterized by increased bone marrow eosinopoiesis and accumulation of activated intestinal eosinophils. IL-5 blockade or eosinophil depletion ameliorated colitis, implicating eosinophils in disease pathogenesis. GM-CSF was a potent activator of eosinophil effector functions and intestinal accumulation, and GM-CSF blockade inhibited chronic colitis. By contrast neutrophil accumulation was GM-CSF independent and dispensable for colitis. In addition to TNF secretion, release of eosinophil peroxidase promoted colitis identifying direct tissue-toxic mechanisms. Thus, eosinophils are key perpetrators of chronic inflammation and tissue damage in IL-23-mediated immune diseases and it suggests the GM-CSF-eosinophil axis as an attractive therapeutic target.
in vivo neutrophil depletion, Flow Cytometry, Immunohistochemistry (paraffin)
Coffelt, S. B., et al. (2015). "IL-17-producing gammadelta T cells and neutrophils conspire to promote breast cancer metastasis" Nature 522(7556): 345-348. PubMed
Metastatic disease remains the primary cause of death for patients with breast cancer. The different steps of the metastatic cascade rely on reciprocal interactions between cancer cells and their microenvironment. Within this local microenvironment and in distant organs, immune cells and their mediators are known to facilitate metastasis formation. However, the precise contribution of tumour-induced systemic inflammation to metastasis and the mechanisms regulating systemic inflammation are poorly understood. Here we show that tumours maximize their chance of metastasizing by evoking a systemic inflammatory cascade in mouse models of spontaneous breast cancer metastasis. We mechanistically demonstrate that interleukin (IL)-1beta elicits IL-17 expression from gamma delta (gammadelta) T cells, resulting in systemic, granulocyte colony-stimulating factor (G-CSF)-dependent expansion and polarization of neutrophils in mice bearing mammary tumours. Tumour-induced neutrophils acquire the ability to suppress cytotoxic T lymphocytes carrying the CD8 antigen, which limit the establishment of metastases. Neutralization of IL-17 or G-CSF and absence of gammadelta T cells prevents neutrophil accumulation and downregulates the T-cell-suppressive phenotype of neutrophils. Moreover, the absence of gammadelta T cells or neutrophils profoundly reduces pulmonary and lymph node metastases without influencing primary tumour progression. Our data indicate that targeting this novel cancer-cell-initiated domino effect within the immune system–the gammadelta T cell/IL-17/neutrophil axis–represents a new strategy to inhibit metastatic disease.
in vivo neutrophil depletion, Flow Cytometry, Immunohistochemistry (paraffin), Immunohistochemistry (frozen)
Finisguerra, V., et al. (2015). "MET is required for the recruitment of anti-tumoural neutrophils" Nature 522(7556): 349-353. PubMed
Mutations or amplification of the MET proto-oncogene are involved in the pathogenesis of several tumours, which rely on the constitutive engagement of this pathway for their growth and survival. However, MET is expressed not only by cancer cells but also by tumour-associated stromal cells, although its precise role in this compartment is not well characterized. Here we show that MET is required for neutrophil chemoattraction and cytotoxicity in response to its ligand hepatocyte growth factor (HGF). Met deletion in mouse neutrophils enhances tumour growth and metastasis. This phenotype correlates with reduced neutrophil infiltration to both the primary tumour and metastatic sites. Similarly, Met is necessary for neutrophil transudation during colitis, skin rash or peritonitis. Mechanistically, Met is induced by tumour-derived tumour necrosis factor (TNF)-alpha or other inflammatory stimuli in both mouse and human neutrophils. This induction is instrumental for neutrophil transmigration across an activated endothelium and for inducible nitric oxide synthase production upon HGF stimulation. Consequently, HGF/MET-dependent nitric oxide release by neutrophils promotes cancer cell killing, which abates tumour growth and metastasis. After systemic administration of a MET kinase inhibitor, we prove that the therapeutic benefit of MET targeting in cancer cells is partly countered by the pro-tumoural effect arising from MET blockade in neutrophils. Our work identifies an unprecedented role of MET in neutrophils, suggests a potential ‘Achilles’ heel’ of MET-targeted therapies in cancer, and supports the rationale for evaluating anti-MET drugs in certain inflammatory diseases.
in vivo neutrophil depletion
Yamada, D. H., et al. (2015). "Suppression of Fcgamma-receptor-mediated antibody effector function during persistent viral infection" Immunity 42(2): 379-390. PubMed
Understanding how viruses subvert host immunity and persist is essential for developing strategies to eliminate infection. T cell exhaustion during chronic viral infection is well described, but effects on antibody-mediated effector activity are unclear. Herein, we show that increased amounts of immune complexes generated in mice persistently infected with lymphocytic choriomeningitis virus (LCMV) suppressed multiple Fcgamma-receptor (FcgammaR) functions. The high amounts of immune complexes suppressed antibody-mediated cell depletion, therapeutic antibody-killing of LCMV infected cells and human CD20-expressing tumors, as well as reduced immune complex-mediated cross-presentation to T cells. Suppression of FcgammaR activity was not due to inhibitory FcgammaRs or high concentrations of free antibody, and proper FcgammaR functions were restored when persistently infected mice specifically lacked immune complexes. Thus, we identify a mechanism of immunosuppression during viral persistence with implications for understanding effective antibody activity aimed at pathogen control.
in vivo neutrophil depletion
Ellis, G. T., et al. (2015). "TRAIL+ monocytes and monocyte-related cells cause lung damage and thereby increase susceptibility to influenza-Streptococcus pneumoniae coinfection" EMBO Rep 16(9): 1203-1218. PubMed
Streptococcus pneumoniae coinfection is a major cause of influenza-associated mortality; however, the mechanisms underlying pathogenesis or protection remain unclear. Using a clinically relevant mouse model, we identify immune-mediated damage early during coinfection as a new mechanism causing susceptibility. Coinfected CCR2(-/-) mice lacking monocytes and monocyte-derived cells control bacterial invasion better, show reduced epithelial damage and are overall more resistant than wild-type controls. In influenza-infected wild-type lungs, monocytes and monocyte-derived cells are the major cell populations expressing the apoptosis-inducing ligand TRAIL. Accordingly, anti-TRAIL treatment reduces bacterial load and protects against coinfection if administered during viral infection, but not following bacterial exposure. Post-influenza bacterial outgrowth induces a strong proinflammatory cytokine response and massive inflammatory cell infiltrate. Depletion of neutrophils or blockade of TNF-alpha facilitate bacterial outgrowth, leading to increased mortality, demonstrating that these factors aid bacterial control. We conclude that inflammatory monocytes recruited early, during the viral phase of coinfection, induce TRAIL-mediated lung damage, which facilitates bacterial invasion, while TNF-alpha and neutrophil responses help control subsequent bacterial outgrowth. We thus identify novel determinants of protection versus pathology in influenza-Streptococcus pneumoniae coinfection.
in vivo neutrophil depletion, Flow Cytometry
Moser, E. K., et al. (2014). "Late engagement of CD86 after influenza virus clearance promotes recovery in a FoxP3+ regulatory T cell dependent manner" PLoS Pathog 10(8): e1004315. PubMed
Influenza A virus (IAV) infection in the respiratory tract triggers robust innate and adaptive immune responses, resulting in both virus clearance and lung inflammation and injury. After virus clearance, resolution of ongoing inflammation and tissue repair occur during a distinct recovery period. B7 family co-stimulatory molecules such as CD80 and CD86 have important roles in modulating T cell activity during the initiation and effector stages of the host response to IAV infection, but their potential role during recovery and resolution of inflammation is unknown. We found that antibody-mediated CD86 blockade in vivo after virus clearance led to a delay in recovery, characterized by increased numbers of lung neutrophils and inflammatory cytokines in airways and lung interstitium, but no change in conventional IAV-specific T cell responses. However, CD86 blockade led to decreased numbers of FoxP3+ regulatory T cells (Tregs), and adoptive transfer of Tregs into alphaCD86 treated mice rescued the effect of the blockade, supporting a role for Tregs in promoting recovery after virus clearance. Specific depletion of Tregs late after infection mimicked the CD86 blockade phenotype, confirming a role for Tregs during recovery after virus clearance. Furthermore, we identified neutrophils as a target of Treg suppression since neutrophil depletion in Treg-depleted mice reduced excess inflammatory cytokines in the airways. These results demonstrate that Tregs, in a CD86 dependent mechanism, contribute to the resolution of disease after IAV infection, in part by suppressing neutrophil-driven cytokine release into the airways.
in vivo neutrophil depletion, Flow Cytometry
Chen, K. W., et al. (2014). "The neutrophil NLRC4 inflammasome selectively promotes IL-1beta maturation without pyroptosis during acute Salmonella challenge" Cell Rep 8(2): 570-582. PubMed
The macrophage NLRC4 inflammasome drives potent innate immune responses against Salmonella by eliciting caspase-1-dependent proinflammatory cytokine production (e.g., interleukin-1beta [IL-1beta]) and pyroptotic cell death. However, the potential contribution of other cell types to inflammasome-mediated host defense against Salmonella was unclear. Here, we demonstrate that neutrophils, typically viewed as cellular targets of IL-1beta, themselves activate the NLRC4 inflammasome during acute Salmonella infection and are a major cell compartment for IL-1beta production during acute peritoneal challenge in vivo. Importantly, unlike macrophages, neutrophils do not undergo pyroptosis upon NLRC4 inflammasome activation. The resistance of neutrophils to pyroptotic death is unique among inflammasome-signaling cells so far described and allows neutrophils to sustain IL-1beta production at a site of infection without compromising the crucial inflammasome-independent antimicrobial effector functions that would be lost if neutrophils rapidly lysed upon caspase-1 activation. Inflammasome pathway modification in neutrophils thus maximizes host proinflammatory and antimicrobial responses during pathogen challenge.
in vivo neutrophil depletion
Deshmukh, H. S., et al. (2014). "The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice" Nat Med 20(5): 524-530. PubMed
Neonatal colonization by microbes, which begins immediately after birth, is influenced by gestational age and the mother’s microbiota and is modified by exposure to antibiotics. In neonates, prolonged duration of antibiotic therapy is associated with increased risk of late-onset sepsis (LOS), a disorder controlled by neutrophils. A role for the microbiota in regulating neutrophil development and susceptibility to sepsis in the neonate remains unclear. We exposed pregnant mouse dams to antibiotics in drinking water to limit transfer of maternal microbes to the neonates. Antibiotic exposure of dams decreased the total number and composition of microbes in the intestine of the neonates. This was associated with decreased numbers of circulating and bone marrow neutrophils and granulocyte/macrophage-restricted progenitor cells in the bone marrow of antibiotic-treated and germ-free neonates. Antibiotic exposure of dams reduced the number of interleukin-17 (IL-17)-producing cells in the intestine and production of granulocyte colony-stimulating factor (G-CSF). Granulocytopenia was associated with impaired host defense and increased susceptibility to Escherichia coli K1 and Klebsiella pneumoniae sepsis in antibiotic-treated neonates, which could be partially reversed by administration of G-CSF. Transfer of a normal microbiota into antibiotic-treated neonates induced IL-17 production by group 3 innate lymphoid cells (ILCs) in the intestine, increasing plasma G-CSF levels and neutrophil numbers in a Toll-like receptor 4 (TLR4)- and myeloid differentiation factor 88 (MyD88)-dependent manner and restored IL-17-dependent resistance to sepsis. Specific depletion of ILCs prevented IL-17- and G-CSF-dependent granulocytosis and resistance to sepsis. These data support a role for the intestinal microbiota in regulation of granulocytosis, neutrophil homeostasis and host resistance to sepsis in neonates.
in vivo MDSC depletion
Deng, L., et al. (2014). "Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice" J Clin Invest 124(2): 687-695. PubMed
High-dose ionizing irradiation (IR) results in direct tumor cell death and augments tumor-specific immunity, which enhances tumor control both locally and distantly. Unfortunately, local relapses often occur following IR treatment, indicating that IR-induced responses are inadequate to maintain antitumor immunity. Therapeutic blockade of the T cell negative regulator programmed death-ligand 1 (PD-L1, also called B7-H1) can enhance T cell effector function when PD-L1 is expressed in chronically inflamed tissues and tumors. Here, we demonstrate that PD-L1 was upregulated in the tumor microenvironment after IR. Administration of anti-PD-L1 enhanced the efficacy of IR through a cytotoxic T cell-dependent mechanism. Concomitant with IR-mediated tumor regression, we observed that IR and anti-PD-L1 synergistically reduced the local accumulation of tumor-infiltrating myeloid-derived suppressor cells (MDSCs), which suppress T cells and alter the tumor immune microenvironment. Furthermore, activation of cytotoxic T cells with combination therapy mediated the reduction of MDSCs in tumors through the cytotoxic actions of TNF. Our data provide evidence for a close interaction between IR, T cells, and the PD-L1/PD-1 axis and establish a basis for the rational design of combination therapy with immune modulators and radiotherapy.
in vivo neutrophil depletion, Flow Cytometry, Immunohistochemistry (frozen)
Huang, L. R., et al. (2013). "Intrahepatic myeloid-cell aggregates enable local proliferation of CD8(+) T cells and successful immunotherapy against chronic viral liver infection" Nat Immunol 14(6): 574-583. PubMed
Chronic infection is difficult to overcome because of exhaustion or depletion of cytotoxic effector CD8(+) T cells (cytotoxic T lymphoytes (CTLs)). Here we report that signaling via Toll-like receptors (TLRs) induced intrahepatic aggregates of myeloid cells that enabled the population expansion of CTLs (iMATEs: ‘intrahepatic myeloid-cell aggregates for T cell population expansion’) without causing immunopathology. In the liver, CTL proliferation was restricted to iMATEs that were composed of inflammatory monocyte-derived CD11b(+) cells. Signaling via tumor-necrosis factor (TNF) caused iMATE formation that facilitated costimulation dependent on the receptor OX40 for expansion of the CTL population. The iMATEs arose during acute viral infection but were absent during chronic viral infection, yet they were still induced by TLR signaling. Such hepatic expansion of the CTL population controlled chronic viral infection of the liver after vaccination with DNA. Thus, iMATEs are dynamic structures that overcome regulatory cues that limit the population expansion of CTLs during chronic infection and can be used in new therapeutic vaccination strategies.
in vivo neutrophil depletion
Richter, K., et al. (2013). "Macrophage and T cell produced IL-10 promotes viral chronicity" PLoS Pathog 9(11): e1003735. PubMed
Chronic viral infections lead to CD8(+) T cell exhaustion, characterized by impaired cytokine secretion. Presence of the immune-regulatory cytokine IL-10 promotes chronicity of Lymphocytic Choriomeningitis Virus (LCMV) Clone 13 infection, while absence of IL-10/IL-10R signaling early during infection results in viral clearance and higher percentages and numbers of antiviral, cytokine producing T cells. IL-10 is produced by several cell types during LCMV infection but it is currently unclear which cellular sources are responsible for induction of viral chronicity. Here, we demonstrate that although dendritic cells produce IL-10 and overall IL-10 mRNA levels decrease significantly in absence of CD11c(+) cells, absence of IL-10 produced by CD11c(+) cells failed to improve the LCMV-specific T cell response and control of LCMV infection. Similarly, NK cell specific IL-10 deficiency had no positive impact on the LCMV-specific T cell response or viral control, even though high percentages of NK cells produced IL-10 at early time points after infection. Interestingly, we found markedly improved T cell responses and clearance of normally chronic LCMV Clone 13 infection when either myeloid cells or T cells lacked IL-10 production and mice depleted of monocytes/macrophages or CD4(+) T cells exhibited reduced overall levels of IL-10 mRNA. These data suggest that the decision whether LCMV infection becomes chronic or can be cleared critically depends on early CD4(+) T cell and monocyte/macrophage produced IL-10.
in vivo neutrophil depletion, Flow Cytometry
Garraud, K., et al. (2012). "Differential role of the interleukin-17 axis and neutrophils in resolution of inhalational anthrax" Infect Immun 80(1): 131-142. PubMed
The roles of interleukin-17 (IL-17) and neutrophils in the lung have been described as those of two intricate but independent players. Here we identify neutrophils as the primary IL-17-secreting subset of cells in a model of inhalation anthrax using A/J and C57BL/6 mice. With IL-17 receptor A knockout (IL-17RA-/-) mice, we confirmed that IL-17A/F signaling is instrumental in the self-recruitment of this population. We also show that the IL-17A/F axis is critical for surviving pulmonary infection, as IL-17RA-/- mice become susceptible to intranasal infection by Bacillus anthracis Sterne spores. Strikingly, infection with a fully virulent strain did not affect IL-17RA-/- mouse survival. Eventually, by depleting neutrophils in wild-type and IL-17RA-/- mice, we demonstrated the crucial role of IL-17-secreting neutrophils in mouse survival of infection by fully virulent B. anthracis. This work demonstrates the important roles of both IL-17 signaling and neutrophils in clearing this pathogen and surviving pulmonary B. anthracis infection.
in vivo neutrophil depletion, Flow Cytometry
Lee, W. B., et al. (2012). "Neutrophils Promote Mycobacterial Trehalose Dimycolate-Induced Lung Inflammation via the Mincle Pathway" PLoS Pathog 8(4): e1002614. PubMed
Trehalose 6,6′-dimycolate (TDM), a cord factor of Mycobacterium tuberculosis (Mtb), is an important regulator of immune responses during Mtb infections. Macrophages recognize TDM through the Mincle receptor and initiate TDM-induced inflammatory responses, leading to lung granuloma formation. Although various immune cells are recruited to lung granulomas, the roles of other immune cells, especially during the initial process of TDM-induced inflammation, are not clear. In this study, Mincle signaling on neutrophils played an important role in TDM-induced lung inflammation by promoting adhesion and innate immune responses. Neutrophils were recruited during the early stage of lung inflammation following TDM-induced granuloma formation. Mincle expression on neutrophils was required for infiltration of TDM-challenged sites in a granuloma model induced by TDM-coated-beads. TDM-induced Mincle signaling on neutrophils increased cell adherence by enhancing F-actin polymerization and CD11b/CD18 surface expression. The TDM-induced effects were dependent on Src, Syk, and MAPK/ERK kinases (MEK). Moreover, coactivation of the Mincle and TLR2 pathways by TDM and Pam3CSK4 treatment synergistically induced CD11b/CD18 surface expression, reactive oxygen species, and TNFalpha production by neutrophils. These synergistically-enhanced immune responses correlated with the degree of Mincle expression on neutrophil surfaces. The physiological relevance of the Mincle-mediated anti-TDM immune response was confirmed by defective immune responses in Mincle(-)/(-) mice upon aerosol infections with Mtb. Mincle-mutant mice had higher inflammation levels and mycobacterial loads than WT mice. Neutrophil depletion with anti-Ly6G antibody caused a reduction in IL-6 and monocyte chemotactic protein-1 expression upon TDM treatment, and reduced levels of immune cell recruitment during the initial stage of infection. These findings suggest a new role of Mincle signaling on neutrophils during anti-mycobacterial responses.
in vivo neutrophil depletion, Immunofluorescence
Edelson, B. T., et al. (2011). "CD8alpha(+) dendritic cells are an obligate cellular entry point for productive infection by Listeria monocytogenes" Immunity 35(2): 236-248. PubMed
CD8alpha(+) dendritic cells (DCs) prime cytotoxic T lymphocytes during viral infections and produce interleukin-12 in response to pathogens. Although the loss of CD8alpha(+) DCs in Batf3(-/-) mice increases their susceptibility to several pathogens, we observed that Batf3(-/-) mice exhibited enhanced resistance to the intracellular bacterium Listeria monocytogenes. In wild-type mice, Listeria organisms, initially located in the splenic marginal zone, migrated to the periarteriolar lymphoid sheath (PALS) where they grew exponentially and induced widespread lymphocyte apoptosis. In Batf3(-/-) mice, however, Listeria organisms remain trapped in the marginal zone, failed to traffic into the PALS, and were rapidly cleared by phagocytes. In addition, Batf3(-/-) mice, which lacked the normal population of hepatic CD103(+) peripheral DCs, also showed protection from liver infection. These results suggest that Batf3-dependent CD8alpha(+) and CD103(+) DCs provide initial cellular entry points within the reticuloendothelial system by which Listeria establishes productive infection.
in vivo neutrophil depletion
Carr, K. D., et al. (2011). "Specific depletion reveals a novel role for neutrophil-mediated protection in the liver during Listeria monocytogenes infection" Eur J Immunol 41(9): 2666-2676. PubMed
Previous studies have suggested that neutrophils are required for resistance during infection with multiple pathogenic microorganisms. However, the depleting antibody used in those studies binds to both Ly6G and Ly6C (anti-Gr-1; clone RB6-8C5). This antibody has been shown to deplete not only neutrophils but also monocytes and a subset of CD8(+) T cells. Recently, an antibody against Ly6G, which specifically depletes neutrophils, was characterized. In the present study, neutrophils are depleted using the antibody against Ly6G during infection with the intracellular bacterium Listeria monocytogenes (LM). Our data show that neutrophil-depleted mice are much less susceptible to infection than mice depleted with anti-Gr-1. Although neutrophils are required for clearance of LM, their importance is more pronounced in the liver and during a high-dose bacterial challenge. Furthermore, we demonstrate that the protection mediated by neutrophils is due to the production of TNF-alpha, but not IFN-gamma. Additionally, neutrophils are not required for the recruitment of monocytes or the generation of adaptive T-cell responses during LM infection. This study highlights the importance of neutrophils during LM infection, and indicate that depletion of neutrophils is less detrimental to the host than depletion of all Gr-1-expressing cell populations.
in vivo neutrophil depletion, Flow Cytometry
Bamboat, Z. M., et al. (2010). "Conventional DCs reduce liver ischemia/reperfusion injury in mice via IL-10 secretion" J Clin Invest 120(2): 559-569. PubMed
TLRs are recognized as promoters of tissue damage, even in the absence of pathogens. TLR binding to damage-associated molecular patterns (DAMPs) released by injured host cells unleashes an inflammatory cascade that amplifies tissue destruction. However, whether TLRs possess the reciprocal ability to curtail the extent of sterile inflammation is uncertain. Here, we investigated this possibility in mice by studying the role of conventional DCs (cDCs) in liver ischemia/reperfusion (I/R) injury, a model of sterile inflammation. Targeted depletion of mouse cDCs increased liver injury after I/R, as assessed by serum alanine aminotransferase and histologic analysis. In vitro, we identified hepatocyte DNA as an endogenous ligand to TLR9 that promoted cDCs to secrete IL-10. In vivo, cDC production of IL-10 required TLR9 and reduced liver injury. In addition, we found that inflammatory monocytes recruited to the liver via chemokine receptor 2 were downstream targets of cDC IL-10. IL-10 from cDCs reduced production of TNF, IL-6, and ROS by inflammatory monocytes. Our results implicate inflammatory monocytes as mediators of liver I/R injury and reveal that cDCs respond to DAMPS during sterile inflammation, providing the host with protection from progressive tissue damage.
- Mus musculus (House mouse),
- Cell Biology
Peripheral monocytes and neutrophils promote photoreceptor cell death in an experimental retinal detachment model.
In Cell Death & Disease on 16 December 2023 by Maidana, D. E., Gonzalez-Buendia, L., et al.
PubMed
Photoreceptor cell death and immune cell infiltration are two major events that contribute to retinal degeneration. However, the relationship between these two events has not been well delineated, primarily because of an inadequate understanding of the immunological processes involved in photoreceptor degeneration, especially that of peripheral leukocytes that infiltrate the subretinal space and retinal tissues. In this work, we characterized the role of leukocyte infiltration within the detached retina. We observed that CD45+ CD11b+ Ly6G+ neutrophils and CD45+ CD11b+ Ly6G- Ly6C+ monocytes are the predominant peripheral immune cell populations that infiltrate the retinal and subretinal space after detachment. Selective depletion of monocytes or neutrophils using cell-specific targeting is neuroprotective for photoreceptors. These results indicate that peripheral innate immune cells contribute to photoreceptor degeneration, and targeting these immune cell populations could be therapeutic during retinal detachment. © 2023. The Author(s).
- Mus musculus (House mouse)
An unexpected role of neutrophils in clearing apoptotic hepatocytes in vivo.
In eLife on 20 September 2023 by Cao, L., Ma, L., et al.
PubMed
Billions of apoptotic cells are removed daily in a human adult by professional phagocytes (e.g. macrophages) and neighboring nonprofessional phagocytes (e.g. stromal cells). Despite being a type of professional phagocyte, neutrophils are thought to be excluded from apoptotic sites to avoid tissue inflammation. Here, we report a fundamental and unexpected role of neutrophils as the predominant phagocyte responsible for the clearance of apoptotic hepatic cells in the steady state. In contrast to the engulfment of dead cells by macrophages, neutrophils burrowed directly into apoptotic hepatocytes, a process we term perforocytosis, and ingested the effete cells from the inside. The depletion of neutrophils caused defective removal of apoptotic bodies, induced tissue injury in the mouse liver, and led to the generation of autoantibodies. Human autoimmune liver disease showed similar defects in the neutrophil-mediated clearance of apoptotic hepatic cells. Hence, neutrophils possess a specialized immunologically silent mechanism for the clearance of apoptotic hepatocytes through perforocytosis, and defects in this key housekeeping function of neutrophils contribute to the genesis of autoimmune liver disease. © 2023, Cao, Ma, Zhao et al.
- Mus musculus (House mouse),
- Genetics,
- Immunology and Microbiology
Neutrophil extracellular traps and extracellular histones potentiate IL-17 inflammation in periodontitis.
In The Journal of Experimental Medicine on 4 September 2023 by Kim, T. S., Silva, L. M., et al.
PubMed
Neutrophil infiltration is a hallmark of periodontitis, a prevalent oral inflammatory condition in which Th17-driven mucosal inflammation leads to destruction of tooth-supporting bone. Herein, we document that neutrophil extracellular traps (NETs) are early triggers of pathogenic inflammation in periodontitis. In an established animal model, we demonstrate that neutrophils infiltrate the gingival oral mucosa at early time points after disease induction and expel NETs to trigger mucosal inflammation and bone destruction in vivo. Investigating mechanisms by which NETs drive inflammatory bone loss, we find that extracellular histones, a major component of NETs, trigger upregulation of IL-17/Th17 responses, and bone destruction. Importantly, human findings corroborate our experimental work. We document significantly increased levels of NET complexes and extracellular histones bearing classic NET-associated posttranslational modifications, in blood and local lesions of severe periodontitis patients, in the absence of confounding disease. Our findings suggest a feed-forward loop in which NETs trigger IL-17 immunity to promote immunopathology in a prevalent human inflammatory disease. © 2023 Moutsopoulos et al.
- Cancer Research
The Efficacy of Nanoparticle Delivery to Hypoxic Solid Tumors by ciRGD Co-Administration Depends on Neuropilin-1 and Neutrophil Levels.
In Advanced Healthcare Materials on 1 September 2023 by Izci, M., Maksoudian, C., et al.
PubMed
The ability to improve nanoparticle delivery to solid tumors is an actively studied domain, where various mechanisms are looked into. In previous work, the authors have looked into nanoparticle size, tumor vessel normalization, and disintegration, and here it is aimed to continue this work by performing an in-depth mechanistic study on the use of ciRGD peptide co-administration. Using a multiparametric approach, it is observed that ciRGD can improve nanoparticle delivery to the tumor itself, but also to tumor cells specifically better than vessel normalization strategies. The effect depends on the level of tumor perfusion, hypoxia, neutrophil levels, and vessel permeability. This work shows that upon characterizing tumors for these parameters, conditions can be selected that can optimally benefit from ciRGD co-administration as a means to improve NP delivery to solid tumors. © 2023 Wiley-VCH GmbH.
- Mus musculus (House mouse),
- Cancer Research
Intratumor Fusobacterium nucleatum promotes the progression of pancreatic cancer via the CXCL1-CXCR2 axis.
In Cancer Science on 1 September 2023 by Hayashi, M., Ikenaga, N., et al.
PubMed
Intratumor bacteria modify the tumor immune microenvironment and influence outcomes of various tumors. Periodontal pathogen Fusobacterium nucleatum has been detected in pancreatic cancer tissues and is associated with poor prognosis. However, it remains unclear how F. nucleatum affects pancreatic cancer. Here, we compared clinical features with F. nucleatum colonization in pancreatic cancer tissues. F. nucleatum was detected in 15.5% (13/84) of pancreatic cancer patients. The tumor size was significantly larger in the F. nucleatum-positive group than in the negative group. To clarify the biological effect of intratumor F. nucleatum on pancreatic cancer progression, we performed migration/invasion assays and cytokine array analysis of cancer cells cocultured with F. nucleatum. F. nucleatum promoted CXCL1 secretion from pancreatic cancer cells, leading to cancer progression through autocrine signaling. Intratumor F. nucleatum suppressed tumor-infiltrating CD8+ T cells by recruiting myeloid-derived suppressor cells (MDSCs) to the tumor in an F. nucleatum-injected subcutaneous pancreatic cancer mouse model, resulting in tumor progression. Furthermore, tumor growth accelerated by F. nucleatum was suppressed by MDSC depletion or cytokine inhibitors. Intratumor F. nucleatum promoted pancreatic cancer progression through autocrine and paracrine mechanisms of the CXCL1-CXCR2 axis. Blockade of the CXCL1-CXCR2 axis may be a novel therapeutic approach for patients with intratumor F. nucleatum-positive pancreatic cancer. © 2023 The Authors. Cancer Science published by John Wiley & Sons Australia, Ltd on behalf of Japanese Cancer Association.
- FC/FACS,
- Mus musculus (House mouse)
Secretory MPP3 reinforce myeloid differentiation trajectory and amplify myeloid cell production.
In The Journal of Experimental Medicine on 7 August 2023 by Kang, Y. A., Paik, H., et al.
PubMed
Hematopoietic stem cells (HSC) and downstream lineage-biased multipotent progenitors (MPP) tailor blood production and control myelopoiesis on demand. Recent lineage tracing analyses revealed MPPs to be major functional contributors to steady-state hematopoiesis. However, we still lack a precise resolution of myeloid differentiation trajectories and cellular heterogeneity in the MPP compartment. Here, we found that myeloid-biased MPP3 are functionally and molecularly heterogeneous, with a distinct subset of myeloid-primed secretory cells with high endoplasmic reticulum (ER) volume and FcγR expression. We show that FcγR+/ERhigh MPP3 are a transitional population serving as a reservoir for rapid production of granulocyte/macrophage progenitors (GMP), which directly amplify myelopoiesis through inflammation-triggered secretion of cytokines in the local bone marrow (BM) microenvironment. Our results identify a novel regulatory function for a secretory MPP3 subset that controls myeloid differentiation through lineage-priming and cytokine production and acts as a self-reinforcing amplification compartment in inflammatory stress and disease conditions. © 2023 Kang et al.
- In Vivo,
- Mus musculus (House mouse),
- Cardiovascular biology,
- Immunology and Microbiology,
- Pathology
Age-induced alterations of granulopoiesis generate atypical neutrophils that aggravate stroke pathology.
In Nature Immunology on 1 June 2023 by Gullotta, G. S., De Feo, D., et al.
PubMed
Aging accounts for increased risk and dismal outcome of ischemic stroke. Here, we investigated the impact of age-related changes in the immune system on stroke. Upon experimental stroke, compared with young mice, aged mice had increased neutrophil clogging of the ischemic brain microcirculation, leading to worse no-reflow and outcomes. Aged mice showed an enhanced granulopoietic response to stroke that led to the accumulation of CD101+CD62Llo mature and CD177hiCD101loCD62Llo and CD177loCD101loCD62Lhi immature atypical neutrophils in the blood, endowed with increased oxidative stress, phagocytosis and procoagulant features. Production of CXCL3 by CD62Llo neutrophils of the aged had a key role in the development and pathogenicity of aging-associated neutrophils. Hematopoietic stem cell rejuvenation reverted aging-associated neutropoiesis and improved stroke outcome. In elderly patients with ischemic stroke, single-cell proteome profile of blood leukocytes identified CD62Llo neutrophil subsets associated with worse reperfusion and outcome. Our results unveil how stroke in aging leads to a dysregulated emergency granulopoiesis impacting neurological outcome. © 2023. The Author(s), under exclusive licence to Springer Nature America, Inc.
- Cancer Research,
- Immunology and Microbiology
Pleiotrophin drives a prometastatic immune niche in breast cancer.
In The Journal of Experimental Medicine on 1 May 2023 by Ganguly, D., Schmidt, M. O., et al.
PubMed
Metastatic cancer cells adapt to thrive in secondary organs. To investigate metastatic adaptation, we performed transcriptomic analysis of metastatic and non-metastatic murine breast cancer cells. We found that pleiotrophin (PTN), a neurotrophic cytokine, is a metastasis-associated factor that is expressed highly by aggressive breast cancers. Moreover, elevated PTN in plasma correlated significantly with metastasis and reduced survival of breast cancer patients. Mechanistically, we find that PTN activates NF-κB in cancer cells leading to altered cytokine production, subsequent neutrophil recruitment, and an immune suppressive microenvironment. Consequently, inhibition of PTN, pharmacologically or genetically, reduces the accumulation of tumor-associated neutrophils and reverts local immune suppression, resulting in increased T cell activation and attenuated metastasis. Furthermore, inhibition of PTN significantly enhanced the efficacy of immune checkpoint blockade and chemotherapy in reducing metastatic burden in mice. These findings establish PTN as a previously unrecognized driver of a prometastatic immune niche and thus represents a promising therapeutic target for the treatment of metastatic breast cancer. © 2023 Ganguly et al.
- In Vivo,
- Mus musculus (House mouse)
Neutrophil extracellular traps formed during chemotherapy confer treatment resistance via TGF-β activation.
In Cancer Cell on 10 April 2023 by Mousset, A., Lecorgne, E., et al.
PubMed
Metastasis is the major cause of cancer death, and the development of therapy resistance is common. The tumor microenvironment can confer chemotherapy resistance (chemoresistance), but little is known about how specific host cells influence therapy outcome. We show that chemotherapy induces neutrophil recruitment and neutrophil extracellular trap (NET) formation, which reduces therapy response in mouse models of breast cancer lung metastasis. We reveal that chemotherapy-treated cancer cells secrete IL-1β, which in turn triggers NET formation. Two NET-associated proteins are required to induce chemoresistance: integrin-αvβ1, which traps latent TGF-β, and matrix metalloproteinase 9, which cleaves and activates the trapped latent TGF-β. TGF-β activation causes cancer cells to undergo epithelial-to-mesenchymal transition and correlates with chemoresistance. Our work demonstrates that NETs regulate the activities of neighboring cells by trapping and activating cytokines and suggests that chemoresistance in the metastatic setting can be reduced or prevented by targeting the IL-1β-NET-TGF-β axis. Copyright © 2023 Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Immunology and Microbiology
Cholesterol sulfate limits neutrophil recruitment and gut inflammation during mucosal injury.
In Frontiers in Immunology on 4 April 2023 by Morino, K., Kunimura, K., et al.
PubMed
During mucosal injury, intestinal immune cells play a crucial role in eliminating invading bacteria. However, as the excessive accumulation of immune cells promotes inflammation and delays tissue repair, it is essential to identify the mechanism that limits the infiltration of immune cells to the mucosal-luminal interface. Cholesterol sulfate (CS) is the lipid product of the sulfotransferase SULT2B1 and suppresses immune reactions by inhibiting DOCK2-mediated Rac activation. In this study, we aimed to elucidate the physiological role of CS in the intestinal tract. We found that, in the small intestine and colon, CS is predominantly produced in the epithelial cells close to the lumen. While dextran sodium sulfate (DSS)-induced colitis was exacerbated in Sult2b1-deficient mice with increased prevalence of neutrophils, the elimination of either neutrophils or intestinal bacteria in Sult2b1-deficient mice attenuated disease development. Similar results were obtained when the Dock2 was genetically deleted in Sult2b1-deficient mice. In addition, we also show that indomethacin-induced ulcer formation in the small intestine was exacerbated in Sult2b1-deficient mice and was ameliorated by CS administration. Thus, our results uncover that CS acts on inflammatory neutrophils, and prevents excessive gut inflammation by inhibiting the Rac activator DOCK2. The administration of CS may be a novel therapeutic strategy for inflammatory bowel disease and non-steroidal anti-inflammatory drug-induced ulcers. Copyright © 2023 Morino, Kunimura, Sugiura, Izumi, Matsubara, Akiyoshi, Maeda, Hirotani, Sakata, Mizuno, Takahashi, Bamba, Uruno and Fukui.
- IHC-IF,
- Mus musculus (House mouse),
- Biochemistry and Molecular biology,
- Immunology and Microbiology
Chemical mimetics of the N-degron pathway alleviate systemic inflammation by activating mitophagy and immunometabolic remodeling.
In Experimental & Molecular Medicine on 1 February 2023 by Silwal, P., Kim, Y. J., et al.
PubMed
The Arg/N-degron pathway, which is involved in the degradation of proteins bearing an N-terminal signal peptide, is connected to p62/SQSTM1-mediated autophagy. However, the impact of the molecular link between the N-degron and autophagy pathways is largely unknown in the context of systemic inflammation. Here, we show that chemical mimetics of the N-degron Nt-Arg pathway (p62 ligands) decreased mortality in sepsis and inhibited pathological inflammation by activating mitophagy and immunometabolic remodeling. The p62 ligands alleviated systemic inflammation in a mouse model of lipopolysaccharide (LPS)-induced septic shock and in the cecal ligation and puncture model of sepsis. In macrophages, the p62 ligand attenuated the production of proinflammatory cytokines and chemokines in response to various innate immune stimuli. Mechanistically, the p62 ligand augmented LPS-induced mitophagy and inhibited the production of mitochondrial reactive oxygen species in macrophages. The p62 ligand-mediated anti-inflammatory, antioxidative, and mitophagy-activating effects depended on p62. In parallel, the p62 ligand significantly downregulated the LPS-induced upregulation of aerobic glycolysis and lactate production. Together, our findings demonstrate that p62 ligands play a critical role in the regulation of inflammatory responses by orchestrating mitophagy and immunometabolic remodeling. © 2023. The Author(s).
- FC/FACS,
- Mus musculus (House mouse),
- Cardiovascular biology,
- Immunology and Microbiology
Neutrophils drive pulmonary vascular leakage in MHV-1 infection of susceptible A/J mice.
In Frontiers in Immunology on 24 January 2023 by Gong, H. H., Worley, M. J., et al.
PubMed
Lung inflammation, neutrophil infiltration, and pulmonary vascular leakage are pathological hallmarks of acute respiratory distress syndrome (ARDS) which can lethally complicate respiratory viral infections. Despite similar comorbidities, however, infections in some patients may be asymptomatic while others develop ARDS as seen with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections for example. In this study, we infected resistant C57BL/6 and susceptible A/J strains of mice with pulmonary administration of murine hepatitis virus strain 1 (MHV-1) to determine mechanisms underlying susceptibility to pulmonary vascular leakage in a respiratory coronavirus infection model. A/J animals displayed increased lung injury parameters, pulmonary neutrophil influx, and deficient recruitment of other leukocytes early in the infection. Moreover, under basal conditions, A/J neutrophils overexpressed primary granule protein genes for myeloperoxidase and multiple serine proteases. During infection, myeloperoxidase and elastase protein were released in the bronchoalveolar spaces at higher concentrations compared to C57BL/6 mice. In contrast, genes from other granule types were not differentially expressed between these 2 strains. We found that depletion of neutrophils led to mitigation of lung injury in infected A/J mice while having no effect in the C57BL/6 mice, demonstrating that an altered neutrophil phenotype and recruitment profile is a major driver of lung immunopathology in susceptible mice. These results suggest that host susceptibility to pulmonary coronaviral infections may be governed in part by underlying differences in neutrophil phenotypes, which can vary between mice strains, through mechanisms involving primary granule proteins as mediators of neutrophil-driven lung injury. Copyright © 2023 Gong, Worley, Carver, Goldstein and Deng.
- Cancer Research,
- Immunology and Microbiology
Induction of T-helper-17-cell-mediated anti-tumour immunity by pathogen-mimicking polymer nanoparticles.
In Nature Biomedical Engineering on 1 January 2023 by Son, S., Nam, J., et al.
PubMed
The effectivity of cancer immunotherapies is hindered by immunosuppressive tumour microenvironments that are poorly infiltrated by effector T cells and natural killer cells. In infection and autoimmune disease, the recruitment and activation of effector immune cells is coordinated by pro-inflammatory T helper 17 (TH17) cells. Here we show that pathogen-mimicking hollow nanoparticles displaying mannan (a polysaccharide that activates TH17 cells in microbial cell walls) limit the fraction of regulatory T cells and induce TH17-cell-mediated anti-tumour responses. The nanoparticles activate the pattern-recognition receptor Dectin-2 and Toll-like receptor 4 in dendritic cells, and promote the differentiation of CD4+ T cells into the TH17 phenotype. In mice, intra-tumoural administration of the nanoparticles decreased the fraction of regulatory T cells in the tumour while markedly increasing the fractions of TH17 cells (and the levels of TH17-cell-associated cytokines), CD8+ T cells, natural killer cells and M1-like macrophages. The anti-tumoural activity of the effector cells was amplified by an agonistic antibody against the co-stimulatory receptor OX40 in multiple mouse models. Nanomaterials that induce TH17-cell-mediated immune responses may have therapeutic potential. © 2022. The Author(s), under exclusive licence to Springer Nature Limited.
Morphine mediated neutrophil infiltration in intestinal tissue play essential role in histological damage and microbial dysbiosis.
In Gut Microbes on 22 November 2022 by Jalodia, R., Kolli, U., et al.
PubMed
The gut microbial ecosystem exhibits a complex bidirectional communication with the host and is one of the key contributing factors in determining mucosal immune homeostasis or an inflammatory state. Opioid use has been established to induce gut microbial dysbiosis consistent with increased intestinal tissue inflammation. In this study, we investigated the role of infiltrated immune cells in morphine-induced intestinal tissue damage and gut microbial dysbiosis in mice. Results reveal a significant increase in chemokine expression in intestinal tissues followed by increased neutrophil infiltration post morphine treatment which is direct consequence of a dysbiotic microbiome since the effect is attenuated in antibiotics treated animals and in germ-free mice. Neutrophil neutralization using anti-Ly6G monoclonal antibody showed a significant decrease in tissue damage and an increase in tight junction protein organization. 16S rRNA sequencing on intestinal samples highlighted the role of infiltrated neutrophils in modulating microbial community structure by providing a growth benefit for pathogenic bacteria, such as Enterococcus, and simultaneously causing a significant depletion of commensal bacteria, such as Lactobacillus. Taken together, we provide the first direct evidence that neutrophil infiltration contributes to morphine-induced intestinal tissue damage and gut microbial dysbiosis. Our findings implicate that inhibition of neutrophil infiltration may provide therapeutic benefits against gastrointestinal dysfunctions associated with opioid use.
- FC/FACS,
- Mus musculus (House mouse),
- Cancer Research,
- Immunology and Microbiology,
- Neuroscience
GZMKhigh CD8+ T effector memory cells are associated with CD15high neutrophil abundance in non-metastatic colorectal tumors and predict poor clinical outcome.
In Nature Communications on 8 November 2022 by Tiberti, S., Catozzi, C., et al.
PubMed
CD8+ T cells are a major prognostic determinant in solid tumors, including colorectal cancer (CRC). However, understanding how the interplay between different immune cells impacts on clinical outcome is still in its infancy. Here, we describe that the interaction of tumor infiltrating neutrophils expressing high levels of CD15 with CD8+ T effector memory cells (TEM) correlates with tumor progression. Mechanistically, stromal cell-derived factor-1 (CXCL12/SDF-1) promotes the retention of neutrophils within tumors, increasing the crosstalk with CD8+ T cells. As a consequence of the contact-mediated interaction with neutrophils, CD8+ T cells are skewed to produce high levels of GZMK, which in turn decreases E-cadherin on the intestinal epithelium and favors tumor progression. Overall, our results highlight the emergence of GZMKhigh CD8+ TEM in non-metastatic CRC tumors as a hallmark driven by the interaction with neutrophils, which could implement current patient stratification and be targeted by novel therapeutics. © 2022. The Author(s).
- FC/FACS,
- Mus musculus (House mouse),
- Immunology and Microbiology
Mobilization of CD11b+/Ly6chi monocytes causes multi organ dysfunction syndrome in acute pancreatitis.
In Frontiers in Immunology on 28 October 2022 by Wilden, A., Glaubitz, J., et al.
PubMed
Acute pancreatitis (AP) is an inflammatory disorder, the severe form of which is burdened with multi-organ dysfunction and high mortality. The pathogenesis of life -threatening organ complications, such as respiratory and renal failure, is unknown. Organ dysfunction was investigated in a mouse model of AP. The influence of monocytes and neutrophils on multi organ dysfunction syndrome (MODS) was investigated in vivo by antibody depletion. Using real-time-fluorescence and deformability-cytometry (RT-DC) analysis we determined the mechanical properties of neutrophils and monocytes during AP. Furthermore, blood samples of pancreatitis patients were used to characterize severity-dependent chemokine profiles according to the revised Atlanta classification. Similar to AP in humans, severe disease in the mouse model associates with organ dysfunction mainly of lung and kidney, which is triggered by a mobilisation of Ly6g-/CD11b+/Ly6c hi monocytes, but not of Ly6g+/CD11b+ neutrophils. Monocyte depletion by anti-CCR2 antibody treatment ameliorated lung function (oxygen consumption) without interfering with the systemic immune response. RT-DC analysis of circulation monocytes showed a significant increase in cell size during SAP, but without a compensatory increase in elasticity. Patient chemokine profiles show a correlation of AP severity with monocyte attracting chemokines like MCP-1 or MIG and with leukocyte mobilisation. In AP, the physical properties of mobilized monocytes, especially their large size, result in an obstruction of the fine capillary systems of the lung and of the kidney glomeruli. A selective depletion of monocytes may represent a treatment strategy for pancreatitis as well as for other inflammation-related disorders. Copyright © 2022 Wilden, Glaubitz, Otto, Biedenweg, Nauck, Mack, Ribback, Bröker, Rheinbaben, Lerch, Aghdassi, Weiss and Sendler.
- FC/FACS,
- Mus musculus (House mouse)
A dissemination-prone morphotype enhances extrapulmonary organ entry by Cryptococcus neoformans.
In Cell Host & Microbe on 12 October 2022 by Denham, S. T., Brammer, B., et al.
PubMed
Environmental pathogens move from ecological niches to mammalian hosts, requiring adaptation to dramatically different environments. Microbes that disseminate farther, including the fungal meningitis pathogen Cryptococcus neoformans, require additional adaptation to diverse tissues. We demonstrate that the formation of a small C. neoformans morphotype-called "seed" cells due to their colonizing ability-is critical for extrapulmonary organ entry. Seed cells exhibit changes in fungal cell size and surface expression that result in an enhanced macrophage update. Seed cell formation is triggered by environmental factors, including C. neoformans' environmental niche, and pigeon guano with phosphate plays a central role. Seed cells show the enhanced expression of phosphate acquisition genes, and mutants unable to acquire phosphate fail to adopt the seed cell morphotype. Additionally, phosphate can be released by tissue damage, potentially establishing a feed-forward loop of seed cell formation and dissemination. Thus, C. neoformans' size variation represent inducible morphotypes that change host interactions to facilitate microbe spread. Copyright © 2022 The Author(s). Published by Elsevier Inc. All rights reserved.
- Cell Biology,
- Immunology and Microbiology
GSDME deficiency leads to the aggravation of UVB-induced skin inflammation through enhancing recruitment and activation of neutrophils.
In Cell Death & Disease on 1 October 2022 by Chen, Y., Lian, N., et al.
PubMed
Gasdermin E (GSDME)-mediated pyroptosis is induced in keratinocytes of UVB-challenged skin. The role of GSDME in UVB-caused skin damage remains unknown. To explore the role of GSDME in UVB-induced skin inflammation. We compared differences in skin appearance, histological features, keratinocyte death modalities, infiltration of immune cells, and levels of some inflammatory cytokines between Gsdme-/- mice and wild type (WT) mice after UVB exposure. We explored whether keratinocytes contribute to GSDME deficiency-caused aggravation of UVB-induced skin inflammation in GSDME knockdown keratinocyte cultured in vitro and keratinocyte-specific Gsdme conditional knockout mice. We used anti-Ly6G antibody to deplete neutrophils and explore their role in UVB-caused skin damage. Skin damage and neutrophils infiltration were aggravated in UVB-challenged Gsdme-/- mice, compared with UVB-challenged WT mice. Apoptosis and necroptosis, which were initiated together with GSDME-mediated pyroptosis in UVB-challenged WT mice, were not enhanced in UVB-challenged Gsdme-/- mice. Neutrophils activation indicators and its recruiting cytokines were increased in skin tissue of UVB-challenged Gsdme-/- mice. However, GSDME knockdown did not lead to the further increase of mRNA and secretion of TNF-α and IL-6 in UVB-challenged keratinocytes. Skin damage was not aggravated in UVB-challenged Gsdme cKO mice. Neutrophils depletion alleviated UVB-caused skin damage in WT mice and Gsdme-/- mice, and eliminated its aggravation in Gsdme-/- mice. This study demonstrates that GSDME plays a restrictive role in UVB-induced skin damage through inhibiting excessive recruitment and activation of neutrophils in the immune microenvironment in UVB-caused skin inflammation. However, keratinocytes might not contribute to this restrictive function. © 2022. The Author(s).
- Cancer Research
Immuno-genomic profiling of biopsy specimens predicts neoadjuvant chemotherapy response in esophageal squamous cell carcinoma.
In Cell Reports Medicine on 16 August 2022 by Sasagawa, S., Kato, H., et al.
PubMed
Esophageal squamous cell carcinoma (ESCC) is one of the most aggressive cancers and is primarily treated with platinum-based neoadjuvant chemotherapy (NAC). Some ESCCs respond well to NAC. However, biomarkers to predict NAC sensitivity and their response mechanism in ESCC remain unclear. We perform whole-genome sequencing and RNA sequencing analysis of 141 ESCC biopsy specimens before NAC treatment to generate a machine-learning-based diagnostic model to predict NAC reactivity in ESCC and analyzed the association between immunogenomic features and NAC response. Neutrophil infiltration may play an important role in ESCC response to NAC. We also demonstrate that specific copy-number alterations and copy-number signatures in the ESCC genome are significantly associated with NAC response. The interactions between the tumor genome and immune features of ESCC are likely to be a good indicator of therapeutic capability and a therapeutic target for ESCC, and machine learning prediction for NAC response is useful. Copyright © 2022 The Authors. Published by Elsevier Inc. All rights reserved.
- Mus musculus (House mouse),
- Cell Biology,
- Immunology and Microbiology
FGL2-MCOLN3-Autophagy Axis-Triggered Neutrophil Extracellular Traps Exacerbate Liver Injury in Fulminant Viral Hepatitis.
In Cellular and Molecular Gastroenterology and Hepatology on 5 August 2022 by Li, X., Gao, Q., et al.
PubMed
Fulminant viral hepatitis (FVH) is a life-threatening disease, but its pathogenesis is not fully understood. Neutrophil extracellular traps (NETs) were an unrecognized link between inflammation and coagulation, which are 2 main features of FVH. Here, we investigated the role and mechanism of NETs in the pathogenesis of FVH. A mouse model of FVH was established by murine hepatitis virus strain-3 infection. Liver leukocytes of infected or uninfected mice were used for single-cell RNA sequencing and whole-transcriptome sequencing. NETs depletion was achieved using DNase 1. Acetaminophen was used to establish a mouse model of non-virus-caused acute liver failure. Clinically, NETs-related markers in liver, plasma, and peripheral neutrophils were assessed in patients with hepatitis B virus (HBV)-related acute liver injury. Increased hepatic NETs formation was observed in murine hepatitis virus strain-3-infected mice, but not in acetaminophen-treated mice. NETs depletion improved the liver damage and survival rate in FVH by inhibiting hepatic fibrin deposition and inflammation. An adoptive transfer experiment showed that neutrophil-specific fibrinogen-like protein 2 (FGL2) promoted NETs formation. FGL2 was found to directly interact with mucolipin 3, which regulated calcium influx and initiated autophagy, leading to NETs formation. Clinically, increased plasma NETs level was associated with coagulation dysfunction in patients with HBV acute liver injury. Colocalization of FGL2, NETs, and fibrin in liver was observed in these patients. NETs aggravated liver injury in FVH by promoting fibrin deposition and inflammation. NETs formation was regulated by the FGL2-mucolipin 3-autophagy axis. Targeting NETs may provide a new strategy for the treatment of FVH. Copyright © 2022 The Authors. Published by Elsevier Inc. All rights reserved.